Understanding Blood Glucose Monitoring: A Guide for Those with Insulin Resistance
Apr 05, 2025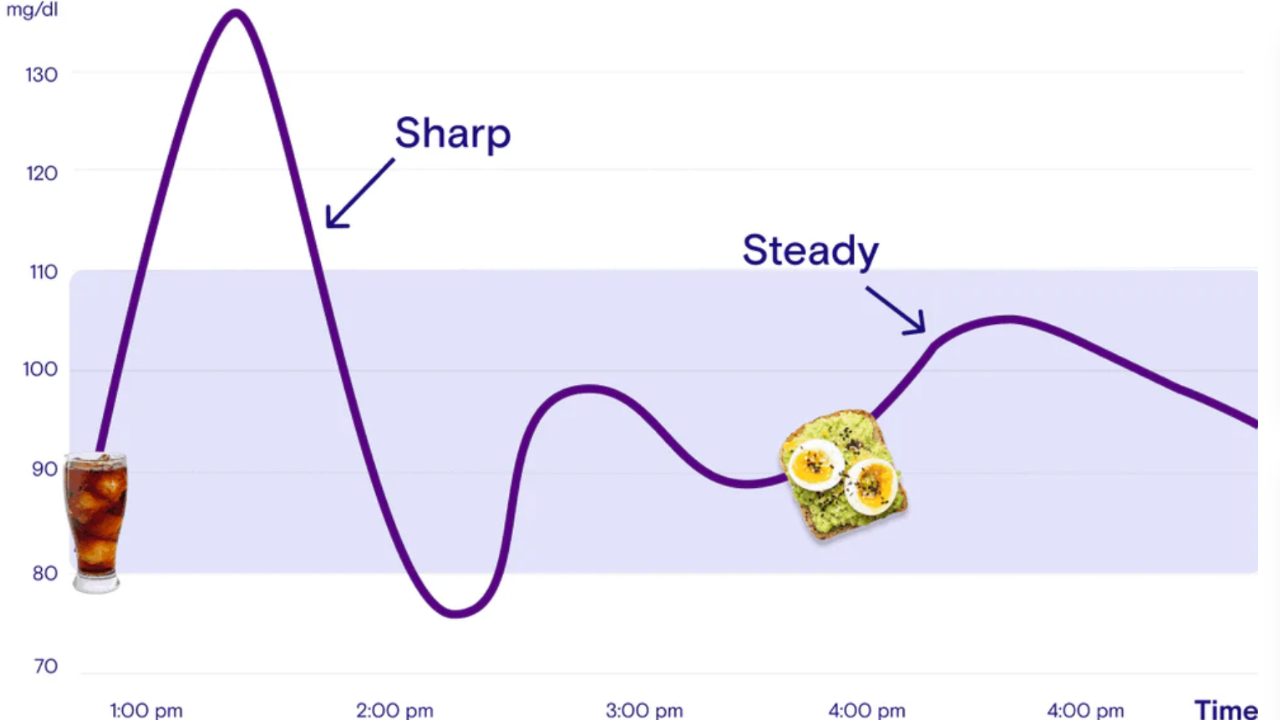
The rollercoaster of blood glucose levels experienced with insulin resistance does more than just affect your physical health—it profoundly impacts your psychological wellbeing. The sudden spikes and subsequent crashes in blood sugar can trigger significant mood disturbances, including depressed mood, heightened irritability and waves of anxiety that seem to come from nowhere. Many individuals struggle with these emotional fluctuations without recognising their physiological origin, often attributing their changing moods to external circumstances or personal shortcomings.
When your body struggles to effectively manage glucose due to insulin resistance, these mood disruptions become part of daily life. The afternoon energy crash that leaves you feeling irritable and unable to concentrate, the morning anxiety that seems disproportionate to your actual stressors, and the persistent low mood that doesn't respond to typical mood-boosting activities—all may be directly linked to unstable blood glucose levels.
Understanding how your individual body responds to various triggers becomes essential not just for metabolic health, but for emotional stability and psychological wellbeing.
Identifying the specific factors—whether they're certain high-glycemic foods, psychological stress, poor sleep quality, or insufficient physical movement—that cause your personal glucose fluctuations provides a powerful tool for mood regulation and overall wellbeing.
This introductory guide aims to help you establish effective blood glucose monitoring practices, allowing you to connect your metabolic patterns with your mood states. By tracking these connections, you'll gain insight into how stress affects your glucose levels, which foods trigger problematic spikes for your unique physiology, how sleep quality influences your morning glucose readings, and how various forms of movement can stabilise both your blood sugar and your emotional state.
Regular monitoring creates a personalised roadmap for managing insulin resistance that extends beyond physical health metrics to enhance your psychological functioning and quality of life. The awareness gained through systematic observation empowers you to make informed choices that support both metabolic and emotional balance.
Why Monitor Blood Glucose?
When you have insulin resistance, your cells don't respond properly to insulin, causing glucose to remain in your bloodstream rather than being absorbed into your cells. Over time, this can lead to consistently elevated blood glucose levels, potentially progressing to type 2 diabetes if left unmanaged.
Regular monitoring allows you to:
Observe how different foods affect your glucose levels and subsequent mood Understand how exercise influences your metabolism and emotional stability Identify stress-related glucose spikes that may trigger anxiety or irritability Track sleep quality correlations with morning mood and glucose readings Document improvements in both metabolic markers and psychological wellbeing as you implement lifestyle changes Provide your healthcare team with comprehensive data connecting physiological and psychological patterns
Getting Started with Glucose Monitoring
There are several methods available for monitoring blood glucose levels. The traditional method involves using a glucose meter, lancet device and test strips to perform a finger prick test. More recently, continuous glucose monitoring (CGM) systems have become increasingly accessible, offering real-time data without frequent finger pricks.
For those new to glucose monitoring, I recommend starting with a standard glucose meter. These are more affordable and provide sufficient data points for establishing baseline awareness. A standard approach includes checking:
Fasting glucose (first thing in the morning) Pre-meal glucose (before each main meal) Post-meal glucose (1-2 hours after eating) Readings during notable mood changes
Once you're comfortable with the process and understand your patterns, you might consider a CGM system for more detailed insights into how glucose fluctuations correlate with mood states throughout the day.
Understanding Your Numbers
Blood glucose readings are typically measured in millimoles per litre (mmol/L) in Australia. While target ranges can vary based on individual factors, general guidelines for adults with insulin resistance include:
Fasting/pre-meal: 4.0-5.5 mmol/L Post-meal (2 hours): <7.8 mmol/L
It's important to note that these ranges may differ based on your specific circumstances. Your healthcare provider can help establish personalised targets for your situation.
Interpreting Glucose Patterns
A single high reading provides limited information, but patterns offer meaningful insights. Pay particular attention to:
Fasting hyperglycaemia: Consistently elevated morning glucose levels may indicate the dawn phenomenon (early morning hormone surges) or worsening insulin resistance. These elevated levels often correlate with morning anxiety and irritability.
Post-prandial spikes: Sharp increases after meals provide information about your carbohydrate sensitivity and metabolic flexibility. Rapid spikes followed by crashes frequently trigger irritability, difficulty concentrating, and sudden mood changes.
Gradual daily increases: If your levels climb throughout the day, this may suggest cumulative dietary influences or stress-related factors that often parallel declining mood and increasing tension.
Recovery time: The duration it takes for glucose to return to baseline after a spike reflects your metabolic efficiency and often coincides with how quickly your mood stabilises after a fluctuation.
Lifestyle Modifications Based on Monitoring Data
Your glucose monitoring becomes particularly valuable when you use it to inform lifestyle adjustments:
Nutritional approaches: Experiment with meal composition, timing and food combinations. Many people discover that pairing carbohydrates with protein, fat and fibre not only modulates glucose responses but also prevents the mood crashes that follow high-glycaemic meals.
Movement strategies: Even short walks after meals can significantly improve glucose handling. Your monitor will show you the glycaemic benefits of various activities, while your mood tracking may reveal emotional benefits that parallel these metabolic improvements.
Stress management: Chronic stress elevates cortisol, which can increase blood glucose. Monitoring may reveal stress-related patterns that respond well to mindfulness practices, with improvements in both glucose stability and emotional regulation.
Sleep optimisation: Poor sleep quality impairs insulin sensitivity. Morning glucose readings often reflect sleep disturbances from the previous night, frequently accompanied by irritability and reduced stress tolerance.
Practical Monitoring Tips
Maintaining consistent monitoring practices ensures more reliable data:
Standardise your approach: Check at similar times each day when possible.
Keep detailed notes: Record food intake, physical activity, stress levels, mood states and sleep quality alongside your readings.
Look for trends rather than fixating on individual readings: Occasional fluctuations are normal; patterns provide more actionable information.
Maintain proper technique: Ensure hands are clean and dry before testing, and follow manufacturer guidelines for your device.
Stay hydrated: Dehydration can concentrate blood glucose readings.
When to Seek Additional Support
While monitoring empowers self-management, certain situations warrant professional guidance:
Consistently elevated readings: If your fasting glucose remains above 5.5 mmol/L despite lifestyle modifications, consult your healthcare provider.
Extreme fluctuations: Wide swings between high and low readings may indicate advancing insulin resistance or other metabolic issues.
Unexplained hypoglycaemia: Readings below 4.0 mmol/L without clear cause should be discussed with your healthcare team.
Signs of diabetes-related complications: Numbness, blurred vision, slow-healing wounds or recurrent infections should prompt immediate medical attention.
Persistent mood disturbances: If significant mood issues persist despite improved glucose stability, consider consulting a mental health professional who understands the metabolic-psychological connection.
The Psychological Aspect of Monitoring
The relationship between psychology and metabolism is bidirectional. Glucose monitoring may initially increase awareness of your condition, which some find anxiety-provoking. However, this awareness typically evolves into empowerment as you gain confidence in your ability to influence both your metabolic health and emotional wellbeing through informed choices.
Practice self-compassion throughout this process. Glucose fluctuations reflect complex physiological processes, not personal success or failure. The goal is progress and understanding, not perfection.
Conclusion
Blood glucose monitoring provides invaluable feedback for those managing insulin resistance and its associated mood disruptions. By systematically tracking your levels and correlating them with lifestyle factors and emotional states, you develop personalised insights that support both metabolic and psychological wellbeing.
Remember that glucose monitoring is one component of a comprehensive approach to metabolic wellness. Integration with appropriate nutritional strategies, movement practices, stress management and sleep optimisation creates a foundation for lasting improvements in both physical and mental health.
This journey toward metabolic awareness begins with simple, consistent steps. Each measurement and observation builds your understanding of your unique metabolic profile, empowering increasingly refined choices that support your overall wellbeing and emotional stability.
If you're struggling with the psychological impacts of insulin resistance and would benefit from professional guidance in integrating glucose monitoring with psychological strategies, I invite you to book an appointment here. At Metabolic Psychology, we can develop a personalised approach that addresses both the metabolic and emotional aspects of your health, creating a comprehensive framework for sustainable wellbeing.
Stay connected with news and updates!
Join our mailing list to receive the latest news and updates from our team.
Don't worry, your information will not be shared.
We hate SPAM. We will never sell your information, for any reason.

